The world is facing a critical healthcare challenge: a nursing shortage. This imbalance between the demand for nurses and the available workforce is putting a strain on healthcare systems around the globe. The nursing shortage is not a new phenomenon, but it has worsened in recent years. An aging population, coupled with high nurse burnout and turnover rates, has created a significant gap in nurse availability. The World Health Organization estimates a deficit of 4.5 million nurses worldwide by 2030, with the shortage being particularly acute in low- and middle-income nations.
Key Findings
Listed below are the key findings that summarize the scale and scope of the nursing shortage, providing a basis for a deeper understanding of its implications and the way forward.
-
- The projected job openings for nurses are much higher than the projected addition of new nurses. There are 193,100 projected job openings for registered nurses (RNs) in the US annually until 2032. However, the projected addition of new nurses stands at 177,400 for the decade between 2022 and 2032, which falls short of filling even one year’s expected job openings.
- The shortage is leading healthcare providers to suspend their operations due to inadequate staff. Since February 2023, 42 medical centers across the US have closed entire medical departments or discontinued specific services, with the nursing shortage being a major contributing factor.
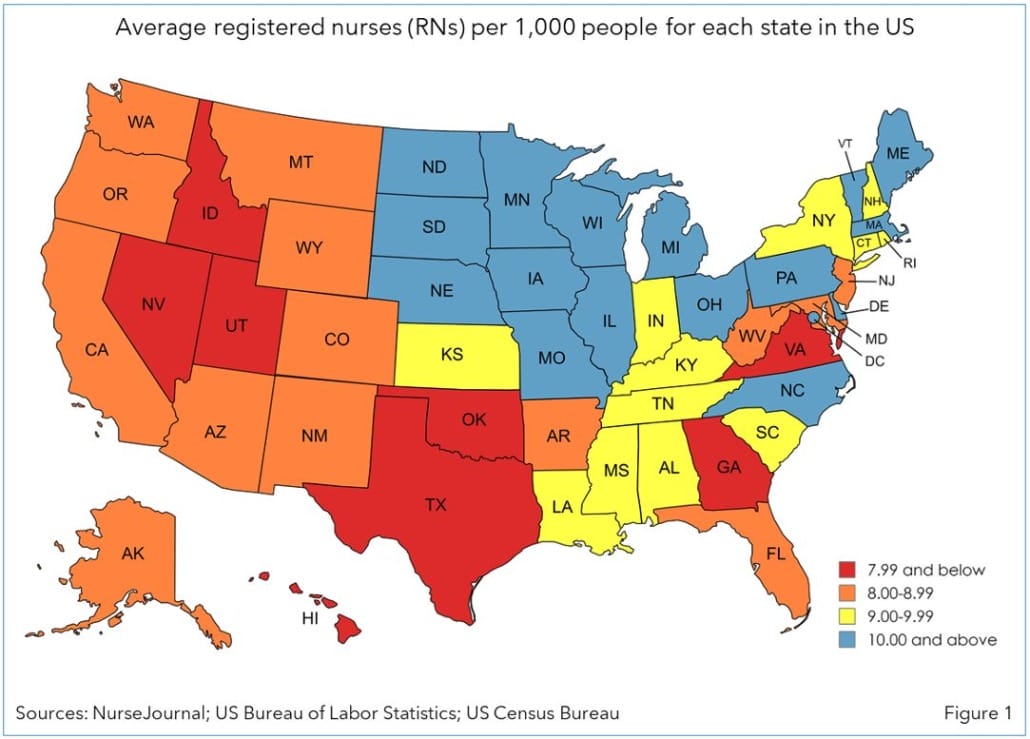
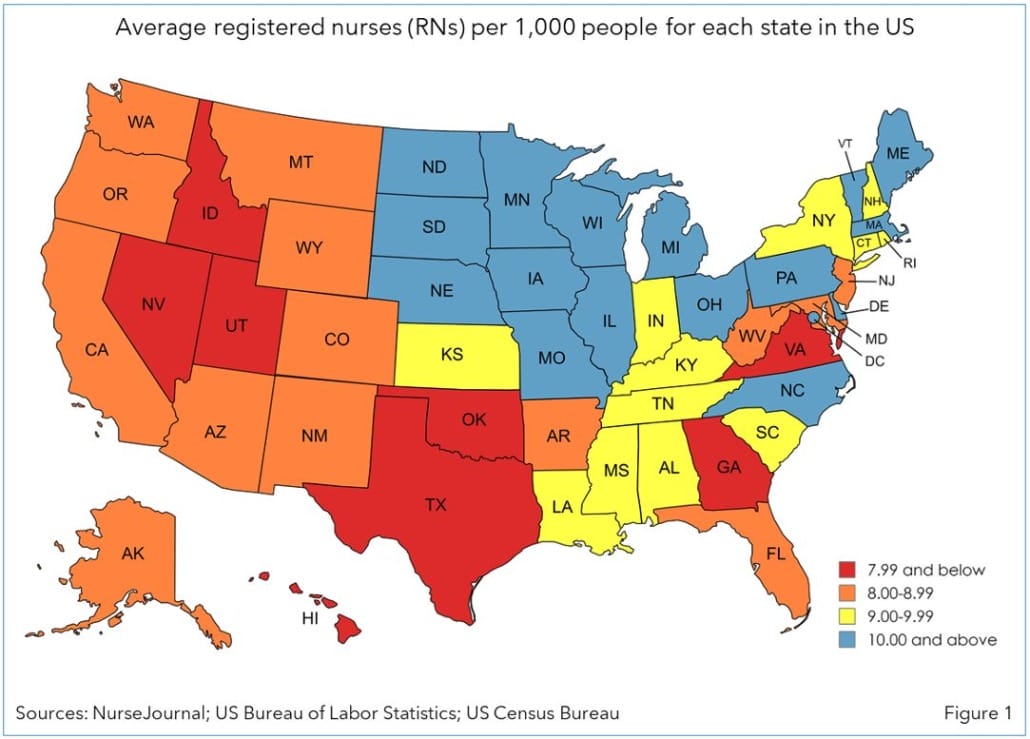
- The nursing ratio (nurses per 1,000 people) is alarmingly low in some US states. Utah, Idaho, and New Mexico have the lowest nursing ratios, at 6.75, 7.06, and 7.53, respectively.
- 42 of the 50 US states are projected to experience a nursing shortage by 2030, with North Dakota being the most affected, meeting only 84% of its anticipated nursing demand.
Impact of the Nursing Shortage
The nursing shortage presents a critical challenge for healthcare systems, with far-reaching consequences that affect both patients and service providers. The scarcity of nurses leads to reduced quality of care as overburdened nurses struggle to manage increasing patient load. This results in delays and diminished support for patient discharge and transition to home care. This situation not only impacts patient outcomes but also drives up healthcare costs, as facilities are forced to rely on costly temporary staffing solutions.
Furthermore, the shortage hampers nurses’ ability to provide adequate patient support, limiting their capacity to effectively assess patient needs, adjust care plans, and offer necessary education and support. Consequently, this leads to lower patient satisfaction, as the limited time and attention that nurses can provide under such strain fail to meet patient expectations.
Dealing with the nursing shortage requires a multipronged approach. This includes bolstering nursing education, improving working conditions to reduce nurse burnout, and implementing innovative staffing strategies to safeguard and prioritize patient care.
Factors Contributing to the Shortage
The nursing shortage results from complex and multifaceted factors, each exacerbating the issue in its own way. These factors collectively highlight the need for strategic interventions to address each contributing element and support the healthcare workforce.
Some of the major factors behind this shortage are as follows:
-
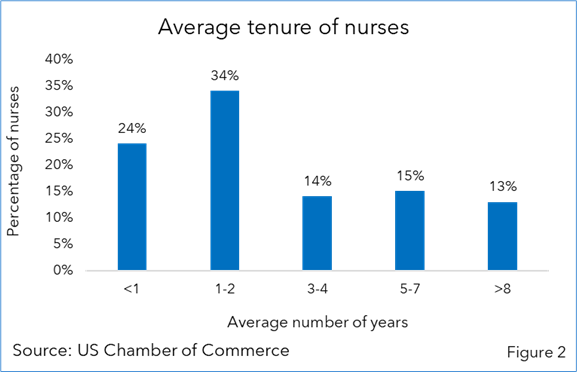
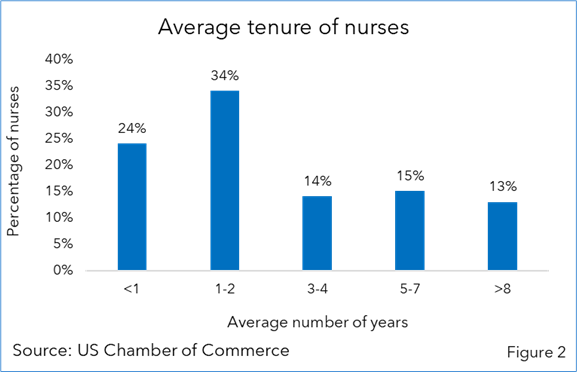
- High turnover: Nursing turnover is a significant issue, varying from a low of 8.8% to a staggering 37% as of February 2023, depending on the region and the clinical field. More than 50% of the nurses leave their jobs within the first two years. This is due to the high burnout, a demanding work environment, emotional exhaustion, and compensation-related concerns.
-
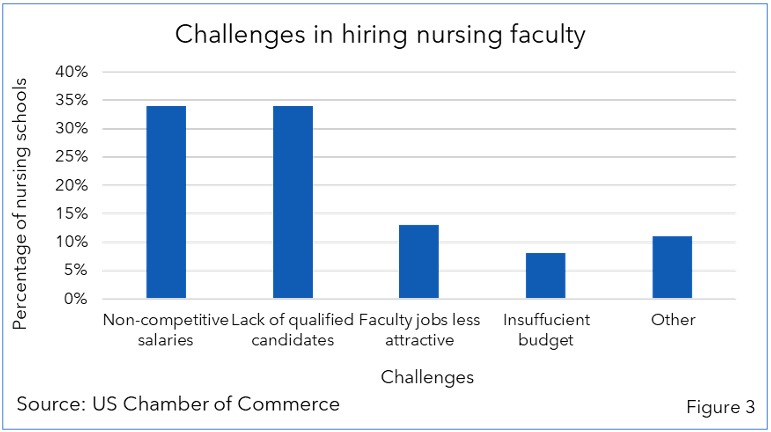
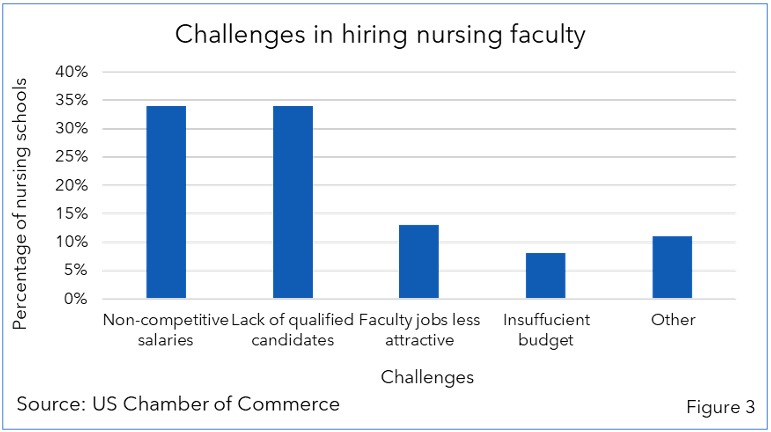
- Limited educational capacity: Due to a shortage of qualified faculty, nursing schools are unable to enroll students to their full capacity. A 2022 study by the National League for Nursing found that 86% of nursing schools had ongoing recruitments for nursing faculty, and 80% of them were facing challenges in their recruitment process.
-
- An aging population: The number of individuals aged 65 and older has reached its highest recorded level in the US. This trend is expected to continue, with the entire baby-boomer generation reaching retirement age by 2030, leading to an increased need for clinical and care management services. Nurses are also part of this aging demographic, with around one million nurses over the age of 50 and nearly 60% of the nurses over the age of 40.
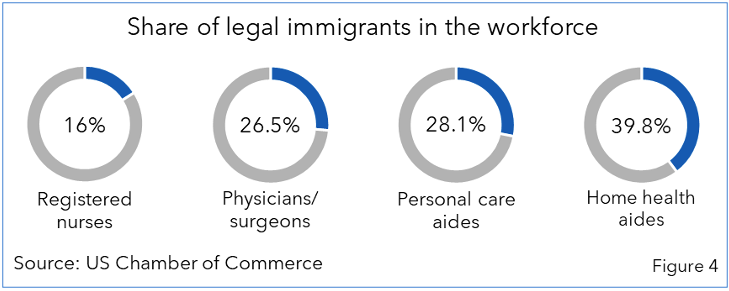
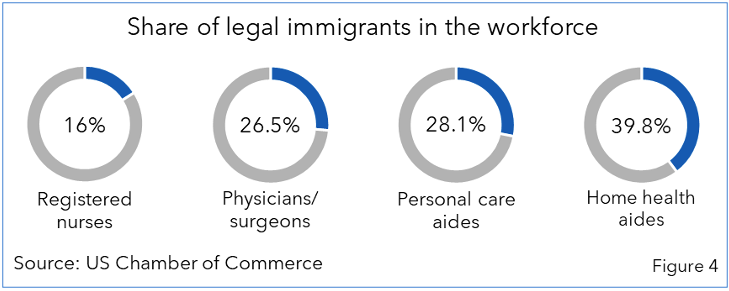
- Lack of employment-based immigration: At present, about 18% of the US healthcare workforce is made up of legal immigrants. International nurses have very limited employment-based immigration options. They have fewer visa options than workers in other industries, hindering the inflow of nurses into the healthcare system.
The Road Ahead: Solutions for the Future
A comprehensive strategy encompassing several key initiatives is essential to address the nursing shortage. When implemented effectively, these solutions can help mitigate the shortage and ensure a robust healthcare system for the future.
-
- Increased investment in nursing education: Expanding nursing school capacity, providing financial aid for nursing students, and creating more faculty positions are crucial steps in catering to the increased demand for nurses. Clinical and care management service providers are establishing their in-house nurse training academies to help nurses get certified by the National Council Licensure Examination for Registered Nurses (NCLEX-RN) and become USRNs. For example, Cognizant has set up the USRN Academy to upskill nurses and help them get registered as USRNs.
- Untapped delivery locations: Service providers can explore countries with high nursing capacity as alternate delivery locations to increase their clinical workforce. Many service providers, including EXL, Sagility, Shearwater Health, and Wipro, are expanding their footprints in locations such as the Philippines, Puerto Rico, Jamaica, Columbia, and South Africa to strengthen their workforce.
- Emerging technologies: Service providers can leverage emerging technologies like AI, ML, automation, and data analytics to enhance their offerings and alleviate the workload of clinical staff. For instance, integrating AI-powered medical scribes can automate routine documentation tasks, freeing nurses to focus on patient care. Similarly, telehealth and remote monitoring solutions can improve patient engagement and reduce the need for in-person visits, while AI-driven analytics can provide valuable insights to inform clinical decisions. For example, Wipro has invested in generative AI with clinical and care management use cases, including case management, conversational voice bots, chatbots, and risk adjustment. Cognizant has also developed generative AI solutions with use cases, including prior authorization, clinical documentation and summarization, and patient education, which significantly reduce the nurses’ workload.
- Improved work environment: To enhance retention, hospitals and healthcare systems can cultivate a nurturing work environment for nurses, provide them with competitive compensation and benefits, and facilitate avenues for professional growth and development. Strategies promoting work-life balance, such as flexible scheduling options, can make nursing a more attractive profession and reduce burnout among practicing nurses.
Conclusion
The nursing shortage transcends a mere quantitative deficit; it represents a fundamental challenge to the integrity of healthcare systems worldwide. A robust nursing workforce is fundamental to achieving universal health coverage where every individual has access to safe, effective care. By investing in nursing education, exploring untapped delivery locations, leveraging emerging technologies, and creating supportive work environments, service providers can take the first steps toward guaranteeing universal access to high-quality healthcare.
By Haril Sadhu, Senior Research Analyst, Avasant, and Aditya Jain, Research Leader, Avasant